What is POTS anyway? I, of course, get this question a lot. I wish I could come up with one straightforward answer that covers all the bases. When I am asked this, my answer certainly varies depending on who I am talking to and, in truth, how tired I am. When I am presented with this question, I have a variety of topics I can discuss in relation to what POTS is. There is, of course, what POTS stands for, all the symptoms it causes, why it is disabling and debilitating, how it changes your day-to-day life, how it is a spectrum, and all of the medical terminology associated with it. Sometimes I try to touch on all of these topics so someone truly interested or someone who is a large part of my life can get the full picture. Other times I say what is easy for me and more understood among the public. I say I have a fainting condition or a “heart issue.” These aren’t untrue; however, they certainly do not cover the extent of the condition and are not entirely accurate from a physiological standpoint. I am constantly torn between whether I should be entirely truthful about this condition and how it affects my day-to-day life. I want and in some ways need people to understand how complex and dynamic POTS and all chronic illnesses are. However, when meeting new people or even continuing relationships with people after being diagnosed with this illness, discussing chronic illness and being fully transparent about what I am dealing with is a turn-off for a lot of people I have come to find. Even those who truly care for you may become uncomfortable when you talk about it. Those diagnosed with chronic conditions grieve the person they were before and have trouble coming to terms with how their illness has changed their lives. Therefore, it is natural for others to also grieve the person, or more so, the abilities of the person they knew before chronic illness, especially since that person isn’t given a prognosis. As a chronically ill person, I don’t know what my illness will look like in the future. Yes, it is chronic, but partial to full remission is a possibility, and I am navigating every day with certain goals in mind. These goals are certainly subject to change as I am still in the process of looking for other treatments, healing my nervous system as a whole (a large feat on its own with little direction from doctors), doing more research, and listening to the stories of others. Therefore, my illness and my mindset are constantly in flux, making it difficult for me to best explain what is wrong with me. However, here is my best attempt at explaining what POTS is.
What is POTS?
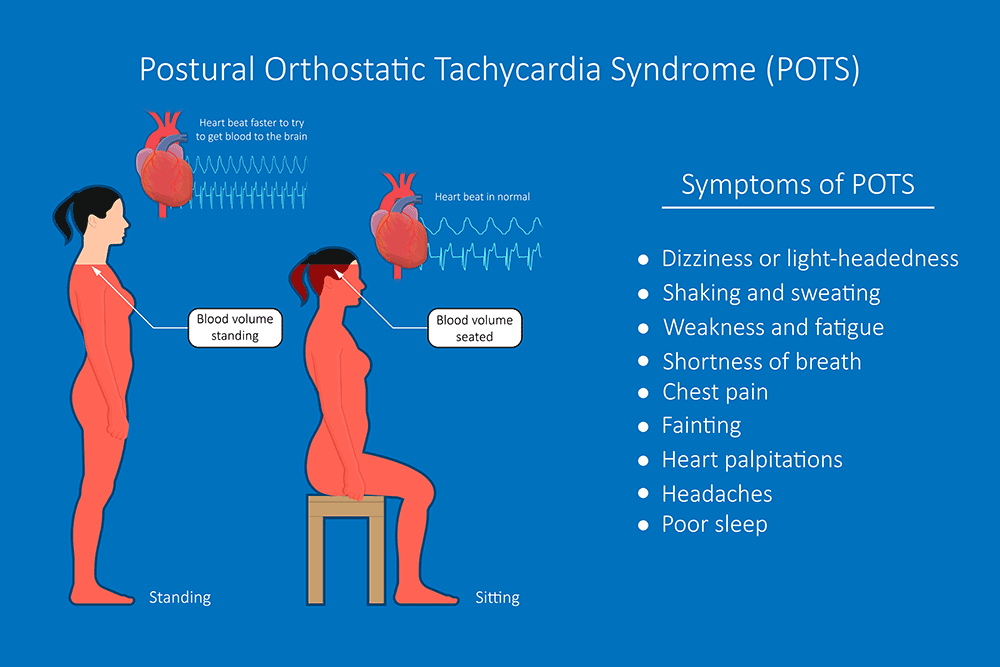
When you google POTS, you will get the following definition from the National Institute of Neurological Disorders and Stroke, as long as Google understands you are talking about a health condition and not containers for plants: “Postural orthostatic tachycardia syndrome (POTS) is one of a group of disorders that have orthostatic intolerance (OI) as their primary symptom. OI is a condition in which an excessively reduced volume of blood returns to the heart after an individual stands up from a lying-down position.” The postural component refers to when one stands up from lying down or sitting, however, it’s possible to have symptoms lying down even with no movement. You may even trigger symptoms with other postural changes or movements, such as reaching your arms above your head, turning your head fast, looking up at the sky, rolling over in bed, coughing, laughing, crying, and even eating. Orthostatic intolerance can also occur because of other positions that aren’t necessarily just standing. With POTS, your blood can pool in multiple different spots in your body, not just your legs and feet. Pooling in the abdomen, arms, and hands is also possible.
Diving Into The Science of it all
Broadly speaking, POTS is a form of dysautonomia, or dysfunction of the autonomic nervous system, which is an extension of the peripheral nervous system, encompassing both the parasympathetic and sympathetic nervous systems. The autonomic nervous system is responsible for controlling involuntary physiological processes. The sympathetic nervous system controls those related to “fight or flight,” while the parasympathetic nervous system controls those related to “rest and digest.” With POTS, the processes associated with the sympathetic nervous system are being signaled inappropriately, especially when one stands. When someone with POTS stands, their nervous system signals their heart rate to increase, not their blood pressure, which may cause a drop in blood pressure for some. People with POTS live in a somewhat perpetual state of fight or flight. That is why POTS symptoms do not only happen with a postural change and why adrenaline rushes are a common symptom. The hormones epinephrine and norepinephrine play a large role in the tachycardia and panic that are felt with POTS. These two hormones are released in excess to try and compensate for the blood pooling in vessels below the heart. More research is needed to be conclusive regarding exactly what is occurring in the body chemically and physically with POTS.
Subtypes?
More recently, it has been proposed that there are subtypes of POTS. It is likely that most with POTS have multiple or even all three subtypes all at once, or flow in and out of each. These subtypes are usually tied to what one believes “caused” their POTS or at least triggered it from its underlying state. For some, there are comorbid conditions such as Ehlers-Danlos syndrome, Mast Cell Activation Syndrome, Lyme disease, and other chronic conditions that are likely linked to their POTS. For others, viruses or infections may lead to the development of POTS. COVID-19 has been linked to many cases of POTS and dysautonomia over the past few years. It also seems to develop following physical trauma from things like surgeries and car accidents. Reverting to the subtypes, there are hyperadrenergic, hypovolemic, and neuropathic subtypes. Hyperadrenergic is typically characterized by a spike in norepinephrine upon standing and may be associated with blood pressure spikes upon standing as well. The hypovolemic subtype is characterized by low blood volume. The neuropathic subtype is characterized by small nerve fiber damage in the fibers that regulate vessel constriction in the limbs and abdomen. I was initially going to include the symptoms that best fit within each subtype, although it is my personal opinion that because many people have a handful of symptoms from multiple categories, it can be confusing and time-consuming to try and assign yourself solely to one type. This is not to say there aren’t some who fit into one subtype, because there are, and some POTS patients may only have a few symptoms that directly correlate with one subtype. For those patients, the diagnosis of a specific subtype may be crucial to treatment. For someone who is hypovolemic, they may be told over and over to increase their fluids and electrolytes; however, this may have little to no effect if they are not retaining much of the fluids and already have a low blood volume. They would benefit from IV infusions. Another instance where diagnosing one’s subtype would be crucial is with someone who experiences a large spike in blood pressure upon standing. If this person is given the same spiel that most POTS patients get from a doctor instructing them to consume a ton of sodium, this may make their blood pressure higher, so salt may not be part of their treatment
Circling back to my opinion on understanding the subtypes, it appears that for a lot of us (those I’ve met or whose stories I’ve read), becoming hung up on testing for a certain type may be to no avail and could be very costly in the end. Finding out if you have other medical issues or traumas is seemingly sufficient on its own to dictate the treatment you should receive, as you will need to try and treat what is indirectly influencing your dysautonomia if possible. However, for those who do not find any other issues or contributors to their POTS, it can be a very difficult start to finding treatment. This is essentially how I started. Naturally, once I found out about the subtypes, I became obsessed with finding out what subtype I had. I figured that had to be the answer to why I was so debilitated despite having tried multiple medications, increasing my salt according to blood pressure and fluid retention, wearing compression gear, etc. For me, I knew I was not hypovolemic because I had had many blood tests, and receiving IV fluids did not seem to do much. At this point, I don’t know if I have any nerve damage or inappropriate levels of norepinephrine. However, even if I did have either or both of those things, my treatment options would be relatively similar. From what I have learned in the course of a little over a year, once you rule out other chronic conditions and, of course, heart issues, treatment is a matter of trial and error and weighing things like costs, side effects, and time consumption with the potential benefits. I think it is likely that I have increased levels of norepinephrine because adrenaline rushes are a major symptom for me, and although I do not have spikes in blood pressure when I stand, I do face blood pressure spikes during some adrenaline rush episodes, even while sitting or lying down. With this knowledge, I knew to try a heart rate medication that would be effective in combating the extreme tachycardia without affecting my blood pressure much.
Medication
As a POTS patient, you will likely be introduced to beta blockers. These are used to treat anxiety and high or low blood pressure, as well as to prevent heart attacks. Being put on medication for electrical or structural heart issues may seem scary since POTS is a disorder of your nervous system that effects your heart rather than an actual heart condition. However, because it affects the signaling of your heart rate and blood pressure, beta-blockers work to block adrenaline and widen blood vessels, which helps combat that fight or flight response and the spiked heart rate upon standing because it reduces the amount of blood pooling. I take metoprolol tartrate twice daily. Metoprolol is a selective beta blocker, meaning it works more directly on the heart than other areas of the body. Metoprolol does lower blood pressure and heart rate, but for me, it does not seem to affect my blood pressure much. My blood pressure typically remains the same when I stand, and I only have certain bouts of low and high blood here and there that seem unrelated to the medication I, therefore, do not have orthostatic hypotension (at least not currently) and don’t require medication to raise my blood pressure.
There is a relatively newer medication that has been deemed a “miracle medication” for some with POTS called Ivabradine or Corlanor. This is the most recent medication I tried, along with continuing my beta blocker, and I have been taking it for almost a year now. Though there is no single medication that will simply rid you of your POTS symptoms and tachycardia for good, Corlanor lowers my heart rate, allowing me to function better. It was the first medication in which I noticed a significant change in heart rate. It does take time to really start to make a difference, however. If I am completely honest, I am not sure if I should still be on Metoprolol along with Corlanor or if I should just seek to increase my dose of Corlanor and drop the beta blocker altogether. Though it has been slightly over a year since I was diagnosed with this condition, I have yet to find a doctor who is knowledgeable about POTS beyond a diagnosis. I am waiting to see a POTS specialist in St. Louis, Missouri, named Dr. Kinsella, and hope to receive his opinion on medications.
On the topic of medication and doctors, I would like to share everything I have tried so far and the types of doctors I have seen. Also, I will surely be making a post regarding what I and others have experienced when seeing doctors as women with chronic illnesses and how these experiences can negatively impact one’s ability to heal from this condition.
So aside from the two medications listed earlier, the only other heart/blood pressure medication I tried was diltiazem. This was at a time when I had not yet been diagnosed with POTS but suspected it. I am unsure why this was what I was prescribed, considering I was coming to my cardiologist with constant sinus tachycardia and had yet to notice any changes in blood pressure. This medication is first used to treat blood pressure and chest pain, and second, it may lower your heart rate. I can’t say for sure that this would not be effective at lowering heart rate for some POTS patients because of how sick I was when I first tried it. When I started taking it I had just been suddenly bed-bound for POTS after a year of mold poisoning and an instance involving the consumption of an edible (I highly regret this!) which seemed to be the final trigger, throwing my POTS into the debilitating condition it has been for a year. However, it did not lower my heart rate much at all and seemed to cause some odd side effects. I have seen multiple cardiologists and one electrocardiologist, and all were in agreement with taking a beta blocker and Corlanor to treat the high heart rate and chest pains. I continued to see cardiologists for two reasons: for one, I had to continue ruling out heart issues via heart monitors and echocardiograms plus the occasional EKG, and two, I was hoping to find one who knew about the condition and could take my treatment further than just medications, salt, and water. Unfortunately, I never found one.
Doctors and more doctors
It is interesting and somewhat comical that the doctors who knew the most about the condition and were the most willing to help with treatment were those of functional medicine and chiropractic care. I saw a hormone doctor who knew about the condition and had multiple patients with it. She tested the hormones (cortisol, estrogen, etc.) and minerals in my blood that may have been influencing my POTS. She also gave me options for treating (holistically, of course) some of the other symptoms I experience aside from those that are cardiovascular-related, such as the IBS that arose as a result. Unfortunately for me, I did not have much success with the supplements used to treat the IBS, but I had only tried one thing after all. Above all, she searched for a root cause and suggested the possibility of mold poisoning after I discussed my horrible sinus issues from the year prior and the presence of black mold in some of the dorms I had frequented. The MD specialist I had initially talked to did not see any reason to search for a root cause and did not want to look at the bigger picture. It turns out I do have mycotoxins in my body. At this point, I am unsure about the treatment for the mold, as it is under researched and could potentially cause me more harm than good. Simply knowing that I have mold toxicity does ease my mind somewhat because it offers an explanation for why I became sick so abruptly and gives me more hope for the potential of remission with POTS. The chiropractor I saw was knowledgeable about POTS and created a holistic treatment plan for me, and while I will admit that parts of it seemed useless and I did not see much of a difference, it was nice to at least have someone trying to help me with a plan in mind. Having a doctor who truly sees you as a person with a life-altering condition and who attempts to help you by giving you some sort of treatment plan, even if there is not much they can offer, can influence your body’s ability to heal itself, especially with nervous system dysfunction. Your mental health plays a large role in your physical symptoms and your ability to deal with your condition and continue fighting without letting anxiety and sadness consume you, so it is undeniable that your doctors’ ability to understand, believe, and treat you highly influences your mindset and your ability to stay hopeful. Again, there is much I would like to share regarding doctors and the medical field. I want to discuss how chronic illness is not well understood and treated, resulting in gaslighting, misdiagnosing, and even neglect. I will get into this in another post.
Wrapping up (finally)
To wrap up this considerably long post, this, of course, does not touch on every part of my story in the last year. In all honesty, I have fallen into survival mode many times this past year and so there are times that seem very hazy and I have had times where I couldn’t even think about my illness without freaking out or becoming very upset. I am still recovering from some of the trauma that the early days of my illness caused me, and at present, I still deal with some strong emotions regarding how my life has changed and the pain and discomfort I feel daily. I am by no means an expert on dysautonomia, and though I know my body pretty well as of late, I am still unsure of what to do for myself at times. Having an illness that isn’t visible and not having tangible evidence of what is “wrong” makes my illness feel incredibly foreign at times, especially when I became disabled in a matter of weeks. It is so important that people with dysautonomia or other invisible illnesses receive a diagnosis quickly so that they aren’t made to feel as if they are crazy and worry themselves sick over whether they are experiencing a medical emergency. The time before a diagnosis sticks with you, even if it is just a few weeks. I still question the symptoms I feel at times and worry I am missing something or even second-guess my illness entirely. I believe these posts could be largely helpful to others who are going through or have gone through a time when POTS is very prevalent in their lives. I plan to discuss a large variety of topics and bring positive and hopeful notes to each post. I won’t lie; it may feel as if dysautonomia has a large grasp on your life and trumps your hope and happiness at times, but there is always light at the end of the tunnel. With the right support system, You can live life the way you want to despite your illness; you will just need to adapt and accept change, despite how hard it may be at first. In the thick of it, you may not believe that to be true; I definitely did not at one point and still have trouble doing so. However, I know now that you must keep striving to get better, no matter how many times you are made to believe it seems hopeless. Chronic illness is becoming more prevalent, especially in young people, and awareness is increasing every day. Despite how limited, research is underway to find treatment due to the number of cases resulting from COVID-19.
Positive/helpful note for todays post: You can find a whole community of fellow POTS people on Facebook groups such as dysautonomia international. These can be very helpful tools in searching for doctors, treatments, and reading other peoples stories so you feel less alone. Be careful to not become super caught up in negative posts. People are scared and sad and will post at their worst and also may be nervously speculating about their symptoms being something super serious. Its a good idea to message someone individually if you feel they are similar to you so you can make a chronically ill friend.


Thank you so much for sharing your story! I’ve heard so much about POTS throughout the years and it’s refreshing to hear about it from someone experiencing it. This was so touching and informative to read. ❤️
Hey! Thank you so much for taking the time to read it!
Thank you so much for sharing. I have a friend at the beginning of this journey. I shared your podcast with her and I will share your blog!
Thank you so much!